Positioning and accuracy are becoming just as important in operating rooms all over the world as the actual scalpel. The jackknife prone position, a surgical posture that, despite its tongue-twister name, is remarkably effective for certain procedures, especially in the colorectal and urological domains, is one of the most recent innovations that is gaining popularity. Surgeons are gaining access to deeper anatomical planes with improved control and visibility by lowering the head and feet in relation to the pelvis and angling the hips at about a 90-degree angle.
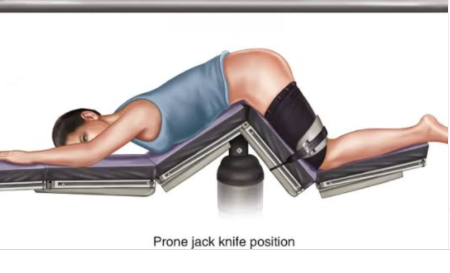
This position is especially advantageous because it makes it easier to access organs like the kidney or adrenal gland from the back, which lessens the invasiveness of intricate operations like laparoscopic nephrectomies. The operating team can reduce tissue tension, improve visualization, and—possibly most importantly—significantly lessen blood loss by placing the patient at this precisely measured angle.
Jackknife Prone Position: Clinical Overview
| Aspect | Detail |
|---|---|
| Also Known As | Kraske Position |
| Body Position | Prone with hips flexed at 90°, head and legs lower than hips |
| Common Uses | Colorectal surgeries, spinal procedures, adrenal gland access, percutaneous nephroscopy |
| Key Advantages | Enhanced surgical access, improved visibility of posterior anatomy |
| Primary Risk Identified | Intraoperative hypotension (low blood pressure during surgery) |
| Supporting Research | Study at Second Affiliated Hospital of Hainan Medical University |
| Notable Study Finding | 2.71x greater odds of hypotension in jackknife vs. lateral position after propensity matching |
| Surgical Recommendations | Extra knee padding, blood pressure monitoring, limited use in elderly hypertensive patients |
| Trusted Reference | Mayo Clinic Education Resource |
Clinical Perspectives and Hazards
Recently, 651 cases involving percutaneous nephroscopy were examined in a landmark study at Hainan Medical University’s Second Affiliated Hospital. The phenomenon was linked to a significantly higher incidence of intraoperative hypotension in patients positioned in the jackknife prone orientation as opposed to those lying laterally. It was primarily attributed to gravitational shifts in blood distribution during surgery. The odds ratio increased to 2.71 following propensity score matching, highlighting the necessity of incredibly transparent patient selection procedures and improved perioperative monitoring.
Age and positioning were found to be statistically significant risk factors by binary logistic regression. Pre-existing hypertension and the length of the surgery were found to be significant predictors of hypotensive episodes in linear regression before and after the match. These results demonstrate how data-driven precision is changing the surgical field.
Using Contemporary Tools to Manage the Position
These days, many of the associated risks—like pressure ulcers, nerve damage, or blood pooling—are being proactively reduced by combining sophisticated padding techniques with ongoing vital monitoring. In addition to improving surgical results, specialized surgical tables with ergonomic supports and adjustable hinges have significantly improved the intraoperative experience for patients.
When applied sparingly and accompanied by attentive intraoperative care, this posture is remarkably adaptable in lowering invasiveness and improving surgical precision. The surgeon gains from shifting the canvas to create safer, better results, much like a sculptor approaches stone from the best angle.
The Prognosis for Surgery on Jackknife Prone
Beyond specialized surgeries, the jackknife prone position might become more widely used in the upcoming years. The method is set to become a mainstay of contemporary minimally invasive procedures thanks to strategic alliances between top hospitals and surgical technology companies. One thing is clear even as research keeps improving our knowledge: careful positioning is becoming the main focus of surgery rather than merely a supporting role.
